Condoms get a bad rap. Most of that is made up of misconceptions though, which is why we’re here to clear them up. The reality is that condoms are an invaluable tool for safer sex. They are currently the only barrier method to effectively prevent the transmission of sexually transmitted infections (STIs). You may be thinking “but I don’t have any STIs!” but in actuality, you can have asymptomatic, yet still transmittable STIs. The only way to ensure you do not have an STI is to get tested regularly. Condoms help prevent the transmission of STIs. It should be noted, there is no shame around STIs; they’re natural and they happen. That being said, most people would prefer to avoid them!
Types of Condoms
When you think of a condom, you probably think about a latex sheath that rolls over any phallic object, be that penis or otherwise. Within this category of external condoms, there are a variety of options that differ in effects and material. There are also internal condoms.
Here are a few of the most common types of condoms:
External
This is the condom you know and (maybe?) love. They are widely available, affordable, and 98% effective when used correctly.
Internal
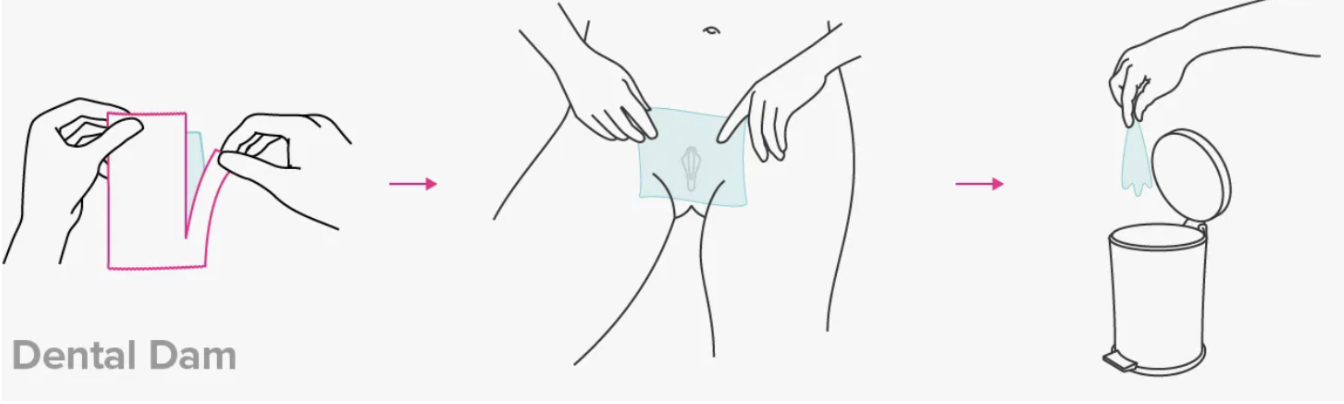
Internal condoms, much less popular than their inverted sibling, are essentially a pouch that's inserted in the vagina or anus. It works like other condoms, except that it's worn on the inside.
Spermicide-coated
There are traditional condoms that are sold with a sperm-killing chemical on them. It is debatable whether the amount is significant enough to make a difference. The best bet, if you are interested in spermicide, would be to use a separate spermicide product in conjunction with condoms.
Polyurethane
Polyurethane condoms are an option for anyone who has a latex allergy. The biggest downside is that these are slightly more prone to breakage which is not a great quality for a condom. This means it is even more important than usual to have an additional contraceptive method on board with these types of condoms. An upside of these condoms is that polyurethane tends to be thinner than latex and may offer a preferable sensation for the person wearing them.
Flavored
Flavored condoms are exactly what they sound like: regular condoms that have flavors. These are best for oral sex, as opposed to vaginal or anal intercourse. As an aside, yes, you should be using condoms even for oral sex. The flavor has the potential to enhance the experience for the giver of oral sex but they should not be used inside any orifice of the body (e.g., vagina or anus) because the ingredients that create the flavor might cause irritation if used internally.
Textured
Textured condoms are also exactly what they sound like: regular condoms but with texture. While the texture offers no protective benefit, it may provide additional pleasure for the recipient of intercourse. It can be fun to experiment with different textures and evaluate how they impact the sexual experience.
Tips
Always make sure your condom fits snugly but not so tightly it might break. Size is a huge factor in condom efficacy.
Do not reuse condoms.
Condoms expire! Regularly check their expiration date to make sure yours are still good to go; if not, they are far more likely to break.
If your condom is not already lubricated, apply lube to the body before insertion to decrease friction (high friction leads to breakage).
Do not keep a condom in your wallet. The heat and friction are a recipe for breakage.
Find a condom that you enjoy the feeling of, or at the very least do not mind. This way, you’ll be far more likely to use them.
Do not use condoms with oil-based lubricant or any other oil-based product like baby oil or Vaseline. They will cause the condom to deteriorate.
Do not wear more than one condom. It’s unnecessary at best and can lead to breakage at worst.
For marathon sessions or longer sexual encounters, switch out condoms about every 30 minutes to prevent breakage.
Happy National Condom Month! Now that you are aware of condom best practices, you can enjoy yourself while practicing safer sex with peace of mind.